
The study included 18 eyes of 18 patients with chronic idiopathic MHs. This retrospective study examined MHs with a duration greater than 1 year, performed by a single surgeon at the Mayo Clinic in Rochester, New York. No face-down positioning surgery for the repair of chronic idiopathic macular holes. Notably, this study did not consider postoperative visual acuity. The study suggests that adhering to strict FDP could improve MH closure rate however, the authors note, patient compliance with FDP is often difficult. For MHs that were greater than 400 µm, the OR was even higher, at 4.361 (95% CI 1.429-13.305, P =. The pooled results showed that the MH closure rate for all surgeries was higher in the FDP group (odds ratio 1.828, 95% CI 1.063-3.143, P =. The meta-analysis included 11 studies including a cumulative 742 surgeries, with 396 patients in the FDP group and 346 patients in the NSP group. In this meta-analysis, the authors reviewed papers that compared strict FDP with nonsupine posturing (NSP) after MH surgery. Comparison of face-down posturing with nonsupine posturing after macular hole surgery: a meta-analysis. This article presents summaries of a sampling of recent publications on this issue.
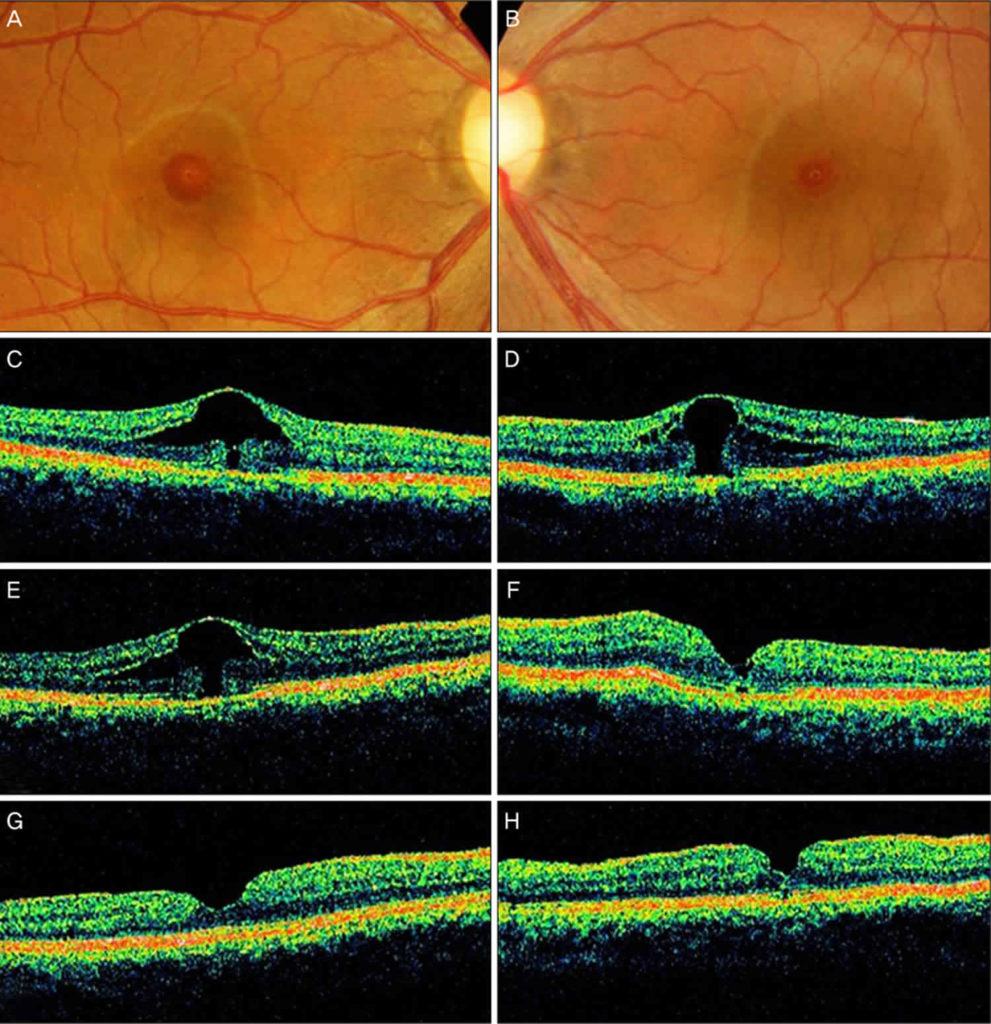
The subject is controversial because there is disagreement over whether or not positioning improves outcomes. Several studies suggest that strict prone positioning may not be necessary after macular hole repair.The authors recap the findings of several recent publications on this topic.There is disagreement regarding whether facedown positioning improves outcomes in macular hole surgery.


 0 kommentar(er)
0 kommentar(er)
